At the beginning of my health experiences, when I was 12 years old, it took about six months to a year to be diagnosed, as we didn’t know there was anything wrong until my appearance started to change. Then, in 2015, I was diagnosed with a secondary condition that I had always had, but it remained dormant until pregnancy. I was shocked by both diagnoses. I had a surgery to remove my thyroids in 2000, then 15 years later, I was told I had thyroid eye disease (TED). The original diagnosis was Graves’ disease with exophthalmos (protrusion of the eyes), and it was assumed resolved when I had the thyroidectomy.
Diagnosed Young, Understood Later
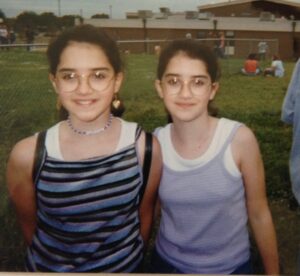
I was diagnosed at such a young age that I didn’t know I needed a community. My family was supportive, and I had a twin sister. That is all I thought I needed. I was so young that I don’t remember what it was like “before” I was ill. At my worst, I was called “bug eyes” and made fun of. From that experience of being made fun of at 12, I saw that I never wanted to be mean to others. Still, I was resilient and moved forward.
In 1998, when I was first diagnosed, the treatment options were limited. It was surgical or radiation. We tried medication to suppress the disease, but it stopped working a couple of years in. We tried symptom management from 2000 to 2020. Then in 2020, we tried biologics. I had 9 out of the 10 side effects from the medication. I was one of the first to report hearing changes from a medication, and those symptoms weren’t even listed on the side effects list. Once I took medication to treat the condition at the source, it was eye-opening to see that typical people don’t have constant sand in their eyes or feel like there is an eyelash flipped the wrong way. You don’t have pressure, and light doesn’t bother you. It was surreal.

The Community I Didn’t Know I Needed
I now follow a tailored treatment approach for TED, which includes diet, symptom management, and infusions. The blend enables me to balance the risks and benefits, thereby improving my quality of life.
Infusions scared me; all I knew of was “chemo” when it came to infusions. I was treated in an infusion center. It was nice to be out of my home, specifically because I didn’t want to create memories for myself being treated at home. I tried to separate that so I could compartmentalize my disease and not fall victim to it. I didn’t like that it felt “clinical”, even though the staff was kind and inviting. Nonetheless, I like that they try to make the experience as comfortable as possible.
Meanwhile, balancing family, work, infusions, and trying to feel human again were real struggles. In 2015, it felt isolating because I was pregnant and going through it while still working. In 2020, I finally found a community, one I didn’t know I needed.
Healing Isn’t Just Physical
When I got a medication that changed my quality of life and then had a disruption due to the Defense Act of 1950, where the government told manufacturing companies to stop making their medications to make vaccines, I became frustrated and became an advocate. Now, knowing many chronic illnesses have no cure, I continue to fight for those living with the condition not to fall victim to their condition but to be empowered to take control of what they can and their mental health by understanding their condition, and living a healthy, balanced life.
Mental health was a massive component of managing my health, but I didn’t know it until I did art therapy. I have been going to traditional therapy for about nine years, and only in 2021 did I find an art therapy program offered by advocacy groups that gave me therapy for 8 weeks at no charge. It showed how much I harbored or was unable to describe at 12 years old. It brought up repressed feelings, but it was a healthy experience.
My condition has shaped my outlook in so many different little ways. As I have been living with the condition for over 27 years, it has ultimately been my whole life. Only recently, over the last four years, have I been able to reflect on how living with the condition has shaped me. Through art therapy and traditional therapy, I have learned tools to communicate more effectively. I no longer minimize my condition or how I felt or am feeling, I am now able to speak confidently and transparently about living with the condition. It takes work and energy to continue moving forward, so I hope others focus on what they can control, which is our thoughts, actions, and reactions to living with chronic conditions.

Our Stories Are Unique, But We’re Not Alone
Someone who does not live with chronic illness can empathize with us, but they never truly understand (nor would I want them to) because if they did, then they would be battling the same challenges. I wish they understood that we are not being lazy when we don’t want to do things; sometimes it is just easier to avoid certain things that can cause symptoms to worsen, and we don’t want to have to explain everything every time. We try not to burden friends, family, and colleagues with things. We still need time to process how to live with it, and it can get exhausting having to explain why we are unable to do things.
Something I want other patients to know is that my story is unique only to me. What that means is everyone’s story is unique, but sharing your story can mean so much to someone else who may not have the words to express what they are feeling. Learning about your condition is essential, but understanding the specific symptoms you have is even more helpful, as it allows you to find tips and strategies to manage the condition. I hope that sharing my story will allow others to feel safe and confident in sharing theirs, as it’s the collective voice that becomes the loudest.
You have to try and error to find what works for you specifically. I believe in self-care. I have been seeing a therapist for over 9 years, and through leadership programs, I have learned how to build confidence in myself through improved communication. This has been extremely helpful for me in advocating for myself. First, to myself, second, to those in my life, and third, to share my story with others in the hope of making a difference in someone else’s life and giving them some hope when they feel lost. I enjoy regular massages, doing stretches at home, and reading a good book. Physically, I tailored my regimens to my providers’ recommendations to help reduce stress and inflammation in my body through routine care, such as using eye drops and wearing a mask while sleeping to help retain moisture in my eyes.

Access Delayed Is Health Denied
Advocacy is a significant part of my story. I became an advocate after having a disruption in the middle of receiving treatment for my health condition. That disruption had major implications for future treatment and resulted in over 18 months of encountering red tape with my commercial payor, the insurance company. Like most autoimmune conditions, the stress and delay in my treatment worsened my symptoms. It was a hard battle to go through, as they were denying medication based on it being experimental.
Medication denials only add an extra layer of difficulty to an already challenging situation. The day before my first infusion, they called me to say that insurance still hasn’t approved it. The approval process was arduous, and had I not had support, I probably would have given up because it felt so burdensome. The back and forth with insurance, followed by the provider needing to provide “extra information,” and the practice being busy, resulted in just delay after delay. Those challenges are particularly complex when you are trying to improve or receive care that could potentially help alleviate your condition. As a healthcare provider, I fortunately knew what questions to ask to make them evaluate their treatment of new medications on the market. I was also lucky that I had the support system to continue to battle them until I finally got the treatment covered.
I wish insurance providers knew it’s their responsibility not to make access even more challenging to gain access to medications or treatments that help those battling chronic or acute health conditions. I have been shocked and disappointed after battling for over 18 months to get the care I needed, spending over 1000 hours on the phone, being sent from one person to another. I have to take copious notes in my industry, and every time I spoke to someone new, the other person did not make notes about my previous calls. That is frustrating because each call states, “This call will be recorded for quality assurance.”
None of my calls were ever heard, so I took the surveys very seriously when I spoke to someone. Insurance is paid for to help cover the costs when people get sick, but right now, it seems like a costly policy that only makes people’s lives harder. Each person I spoke to was nice, but very unhelpful, as they are doing what they are told to push the policy, but they cannot help beyond what they can ask their supervisors.

Why I Speak Up
To Policymakers:
I want policymakers to understand their role in helping people by making healthcare more accessible. I am familiar with the business side of healthcare; however, the mission should always be about serving others, and when done well, you can have a healthy business while delivering excellent patient care. It’s your responsibility, as leaders, to recognize what we can change to help those whom the policies affect. There are many stories out there that feel underrepresented by our policymakers. It would be a game changer if advocacy came from a company that is contracted with companies to help pay for your care. You would not have to fight to get the medication you need, and they would help fight for you to get the treatment you need, which would help reduce the stress of whatever condition you are living with.
To Medical Providers:
I would love medical professionals to understand their role when someone is recently diagnosed with a condition. As providers, we sometimes minimize the condition as we see it every day in our practices. Each patient needs to feel you have enough time for them, so recognize when you are unable to give them the time and reschedule or bring your assistant in to help serve as a go-between to answer questions. I would like providers to know that the patient voice is so powerful because if you let them, they will share with you the most valuable information about their condition to help guide their care.
To Patients, Caregivers, and Advocates:
Patients, providers, advocates, and policymakers all have their own stories. I want to make a difference and help someone think twice before making life more complicated or more challenging for those living with chronic health conditions. Sharing my story has been therapeutic for the little girl inside who always said she was okay because I didn’t want my mom to be scared or my twin sister to worry. I was constantly wanting to make sure I wasn’t a burden to others, and it is only through working in therapy that I have been able to gain my voice back without hesitation or regret.
I want to make a difference in someone’s life, even if I don’t know them personally, so this is why I share my story to help others living with TED not feel isolated, alone, or scared. Connection is key to being human, and no one can truly understand living with a condition until they have experienced it firsthand.

Why Advocacy Organizations Matter
Advocacy organizations can build a community to help people facing similar challenges know there is hope. There is a pathway to feeling “normal” again. We can share stories and not minimize our condition to those not living with the disease. Everyone faces challenges and troubles in their day-to-day lives. I haven’t met one person in my line of work who didn’t have a challenge. Advocacy organizations are a collective group of people who understand both sides, and they fight for you when you can’t find the fight in yourself, and some of them teach you how to be an advocate.
Organizations like the Infusion Access Foundation are critical for the patient voice to spread beyond non-profit organizations. You work with the patient to share their story and raise awareness among policymakers and beyond. Without organizations like yours, certain conditions would be left in the dark. You create a safe and accessible space for people to come, build a community, and share their stories to make a difference. More organizations should strive to build advocacy and community in their missions.
Working with your organization and other nonprofit organizations has impacted my healthcare journey in ways I never expected. Advocacy through organizations has given me an avenue to work through living with a health condition for over 27 years, and it has helped me find the truest version of myself. This impact is lifelong, and I will continue working to help others find their voice.
Healing takes many forms, and no one should have to navigate chronic illness alone or uphill. Through advocacy, connection, and the courage to be seen, patients can help create a system that sees them. Written by Layla Lohmann. Edited in partnership with the Infusion Access Foundation team.






